Does Medicaid Cover Pulse Oximeter
Your doctor can have the test done on you and charge them or your DME can. Patient has chronic lung disease severe cardiopulmonary disease or neuromuscular.

Fingertip Pulse Oximeter Mymedsupplies Com By Geneva Woods Health Supplies
The beneficiary does not meet the criteria listed in.

Does medicaid cover pulse oximeter. Medicare does not cover pulse oximeters. Routine use of oximetry is non-covered. Routine use of oximetry is non-covered.
A pulse oximeter is a covered medical equipment item eligible for reimbursement when used in a personal residence as an alternative to hospitalization to manage the care of oxygen dependent pediatric recipients. 72018 Ohio Department of Medicaid CERTIFICATE OF MEDICAL NECESSITY. Alabama Medicaid Agency Pulse Oximeter Children under 21 years of age and EPSDT eligible PREREQUISTE CRITERIA The following criteria must be met.
Medicare will help pay for oxygen equipment contents and supplies for the delivery of oxygen when all of these conditions are met. It is linked to a processing unit which delivers a read-out indicating an individuals oxygen saturation. Oxygen equipment accessories.
Home pulse oximetry is not covered for the. Some private insurance plans do cover pulse oximetry services. Patient is already approved for supplemental home oxygen systems.
Diseases which isare commonly associated with oxygen desaturation. Medicare will allow payment for oximetry when accompanied by an appropriate ICD-9-CM code for a pulmonary disease s which is commonly associated with oxygen desaturation. Policy For Medicare Members.
Is limited to one month rental or. Not likely as they are not a medical necessity. Early symptoms of coronavirus now can be detected with Oximeter.
Per Medicare guidelines oximeters E0445 and replacement probes A4606 will. For instance Aetnas Medicaid plan in Pennsylvania considers pulse oximetry for home use a coverable service under specific diagnostic criteria such as chronic lung disease. The Wisconsin Medicaid and BadgerCare Update is the first source of program policy and billing information for providers.
Medicare coverage of home oxygen and oxygen equipment under the durable medical equipment DME benefit see 1861 s 6 of the Social Security Act is considered reasonable and necessary only for patients with significant hypoxemia who meet the medical documentation laboratory evidence and health conditions specified in subsections. The additional Group II criteria do not apply to these patients. Raised Toilet Seats Blood Pressure Monitors.
Name Name Name Medicaid ID number Medicaid provider number Medicaid provider number Date of birth NPI NPI Address. Medically necessary reasons for pulse oximetry include. Medicaid will differ from the amount billed to the private payer.
False certification constitutes Medicaid fraud. The daily rental of stationary or portable oxygen systems includes contents. Many people are catching up on these current developments of the.
Although the Update refers to Medicaid recipients all information applies to BadgerCare. Should include an event recorder c. Some things in life you just have to take the responsibility for.
Id like the doctor to write me a script for a new truck to go to the. A trained caregiver should be available to respond to changes in the oxygen saturation. Patient exhibits signs or symptoms of acute respiratory dysfunction such as.
The debate about using oximeter in-home monitoring is still going on in the medical field. Must be ordered by the Members treating physician. The beneficiary does not meet the eligibility requirements listed in.
The pulse oximeter is noninvasive consisting of a sensor attached to an individuals finger nose ear or toe. The home use of oxygen is covered for those members with arterial oxygen partial pressure measurements from 56 to 65 mmHg or oxygen saturation at or above 89 who are enrolled subjects in clinical trials approved by CMS and sponsored by the National Heart Lung and Blood Institute NHLBI. There are a lot of medical professionals who have actually recommended using Oximeter on COVID-19 patients or on regular people to discover if they have the flu or not.
Medicaid and NCHC shall not cover the procedure product or service related to this policy when. This is done by measuring light absorption of oxygenated hemoglobin and total hemoglobin in arterial blood. The following items are only covered under Medicaid Incontinence Supplies.
Identifying Information This section may be completed by the provider Individual Prescriber Provider. Pulse Oximeter for Home Use CommercialMedicareNHMedicaid Policy Guidelines Coverage Criteria. Tachypnea Dyspnea Cyanosis Respiratory distress Confusion Hypoxia 2.
The use of continuous home pulse oximetry. Home pulse oximetry is covered when used to monitor oxygen saturation in order to determine appropriate supplemental oxygen levels. These temporary flexibilities will end the earlier of the cancellation of the North Carolina state of emergency declaration or when the policy modification is rescinded.
41 General Criteria Not Covered. Routine use of oximetry is non-covered. Medicare Part B Medical Insurance covers the rental of oxygen equipment and accessories as durable medical equipment DME that your doctor prescribes for use in your home.
Effective retroactive to March 10 2020 Medicaid and NC Health Choice plans are temporarily covering weight scales and adding a purchase option for portable pulse oximeters. Medicare will allow payment for oximetry when accompanied by an appropriate ICD-9-CM code for a pulmonary disease s which isare commonly associated with oxygen desaturation. Patient must be Medicaid and EPSDT eligible.

Pin On Business Industrial Supplies
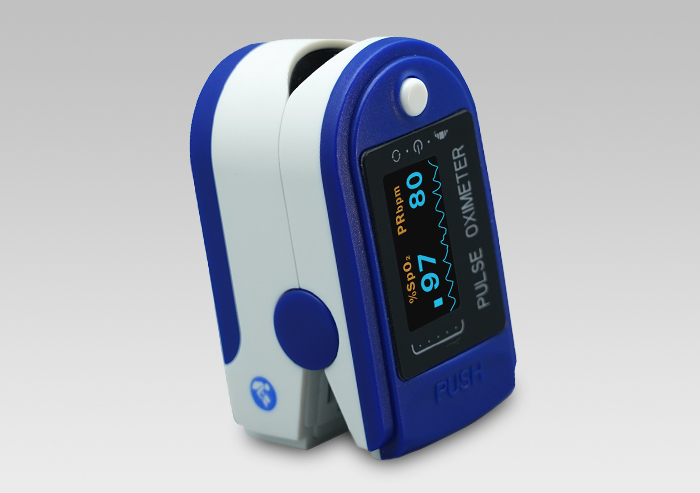
Fingertip Pulse Oximeter Mymedsupplies Com By Geneva Woods Health Supplies
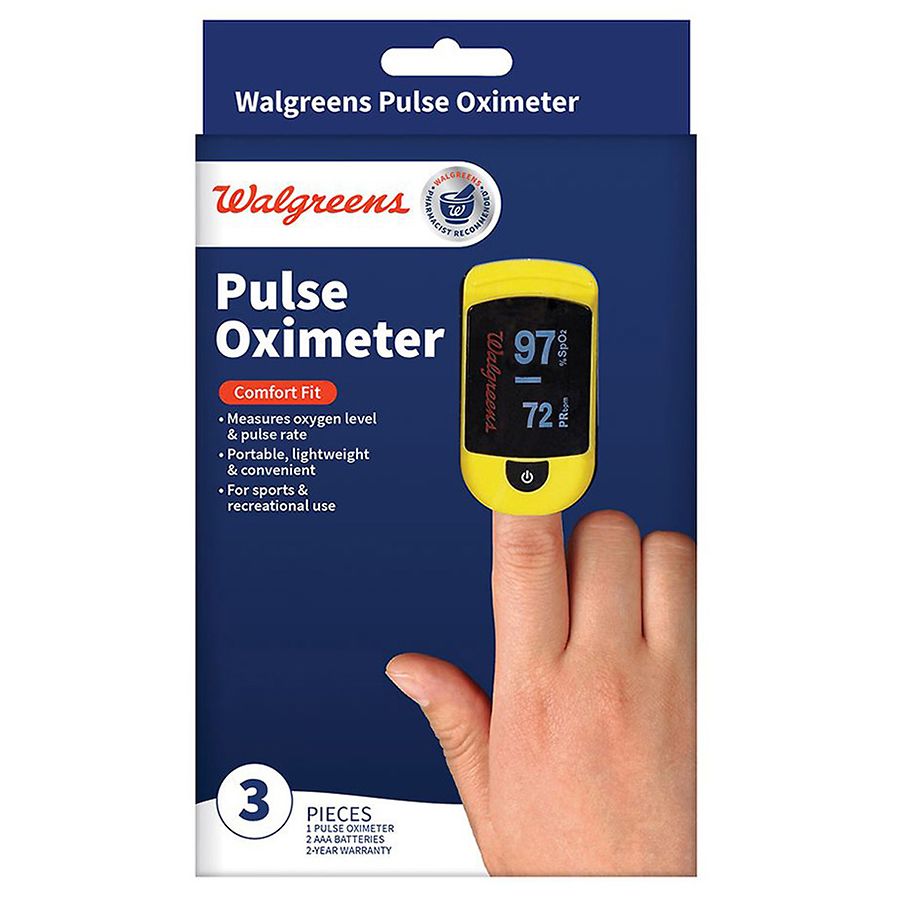
Walgreens Fingertip Pulse Oximeter Walgreens

Chinese Pulse Oximeter For The Finger From Bangood 4k Video Youtube